This talk was presented at the International Pediatric Orthopaedic Symposium in Orlando, Florida last November 2022. My topic was to talk on patients with neuromuscular scoliosis (NMS) who were less than 8 years of age, presenting the argument to do Growing Rod (GR) surgeries, instead of performing a Posterior Spinal Fusion (PSF). My opponent was Dr. Nick Fletcher from Children’s Healthcare of Atlanta, who provided a nice counter-argument presentation for PSF in this patient population.
My side of the debate was an easy one for me to support, specifically to support GR surgeries. I will present the slides of the talk and give some additional information.
The diagnosis of NMS lumps together a wide variety of neuromuscular diagnoses, from cerebral palsy to spina bifida to spinal muscle atrophy, just to name just a few. With these different neuromuscular diseases come a wider variety of medical comorbidities, such as cardiac (heart), pulmonary (lung), and endocrine issues which can impact surgery and the
recovery from surgery. When compared to idiopathic, syndromic, and congenital scoliosis patients, neuromuscular patients are by far the most challenging group of patients.
In NMS the impact on the child can be broken down into two broad groups, orthopaedic and
medical. One main musculoskeletal problem we see in NMS is difficulty in sitting, which can be called “imbalance”, because the pelvis is tipped. When the patient tries to get their bottom onto the seat of their wheelchair they lean severely to the left or the right.
The other main problem we see in NMS is back pain when patients are sitting. The bigger the scoliosis, and the more the pelvis is tipped the higher, the chance of having pain when sitting. This can be a significant problem preventing the children to sit in a car seat, be upright in school and/or be unable to travel any significant distances.
The last bullet point on this slide is about T1-S1 distance, which is a quantitative measurement of the distance from the shoulders to the pelvis. The longer this distance is, the
greater potential lung volume will be.
However, we don’t often know how much distance a single child will need to have no pulmonary problems (pneumonias, shortness of breath, etc…) in adolescence and adulthood. Also, we don’t know the growth potential for any one child. What we do know is that, in general, children with neuromuscular disease do not grow as much as the family history (height of parents and siblings) may predict.
So if a child has NMS, and is less than or under 8 years of age and needs surgery, how do we know if a child should undergo GR or PSF surgery? We know the data to support either surgery, over the other, is poor. The main reason is we don’t know how much T1-S1 distance a child needs at the end of growth or how much potential T1-S1 growth any child may have….. so we need to have discussions, between the surgeon and family/caregivers about the two options, and their benefits, risks, and potential complications.
As indicated on the slide, we need to discuss:
- Number of procedures a family/caregiver is willing to have the child undergo.
- The tolerance of complications, such as implant breakage, implant pull-out and infection.
- The ability of the family/caregivers to be able to deal with complications and need for hospitalizations and procedures, sometimes with short notice.
- The amount of T1-S1 distance a patient may need
- The patient’s pulmonary (lung) status, such as need for supplemental oxygen, tracheostomy or use of a ventilator to breath.
For each child/family/caregiver there is a unique situation for each item #1-#5….and varying degrees. These discussions can take many months or years to come to a decision. Each child and decision is unique.
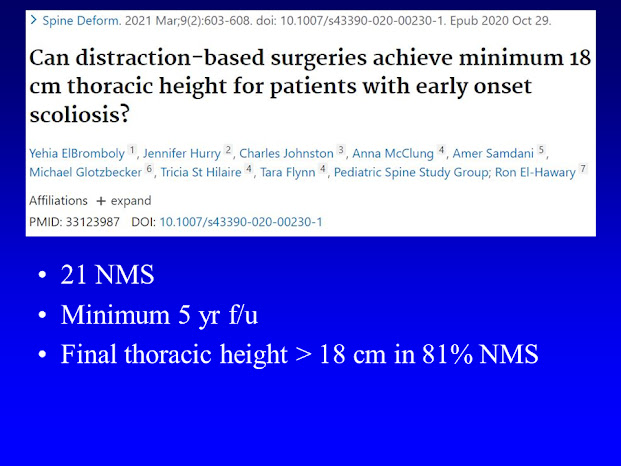
This slide presents a published study from the Pediatric Spine Study Group on the use of GR in NMS. 81% of patients achieved a T1-S1 distance of 18 cm, which is the minimum distance currently believed to be sufficient for asymptomatic pulmonary function though there is scant data to support this position.
Not every scoliosis needs surgery right away. Here is a 9 year old girl with CP. In the first
picture on the left there is severe scoliosis of 81 degrees and pelvic obliquity (tipped pelvis) of 28 degrees (away from being level). Move to the third picture from the left and you see there is kyphosis of 76 degrees (high end of the normal range is 50 degrees). So this young lady has a
severe kypho-scoliosis, a combination of both deformities. This magnitude of deformity typically ends up getting surgery, however see the 2nd from the left and the 4th
from the left pictures and you see how flexible she is! The scoliosis goes down to 45 degrees and the kyphosis down to 28 degrees! Based on this information we can treat nonsurgically with bracing and wheelchair modifications. Eventually she will need PSF surgery but it will be just one surgery… and not several!
The goals for surgery mirror the topics which should be part of preoperative discussions:
- Improve pelvic obliquity
- Improve scoliosis and/or kyphosis
- Increase T1-S1 distance
- No complications. It is important to point out GR constructs will have more complications than PSF due to the nature of the GR constructs (stiff metal, relatively flexible spine) and the need to convert these patients to a final, definitive at or near the end of skeletal growth.
- Durable; minimal reoperations. To this point, traditional growing rods (TGRs) will need more surgeries than magnetically-controlled growing rods (MCGRs). This is because the MCGRs can be lengthened in the office without sedation, while TGRs need to be lengthened in the OR under general anesthesia (about every 6 months). Hence we try very hard to place MCGR, but sometimes patients size and deformity prevents us from placing them, and we have to place TGRs.
The correction forces of GRs is demonstrated on this slide. A car jack, which lifts a car off the ground, has two points it is distracting against, the ground and the car. In GRs we need to establish two point to distract against, and these need to be over the area of the spine deformity in order to correct the deformity. So there are two foundations which need to be
created:
- Cranial (Upper)
- Caudal (Lower)
- Cranial fixation points can be ribs or the spine.
- Caudal fixation points can be spine, iliac crest or the sacrum-pelvis
Cranial or upper fixation point option are the ribs, and there are many of them on each side of the chest. After using them for many years, it appears these are likely a better option than the spine in children under 7 years of age. When these are used 3-4 ribs should be used for each rod, to minimize the occurrence of the rib hooks pulling through the ribs.
This slide demonstrates two points of interest: the use of spine fixation (pedicle screws) cranially and the use of only one rod.
- The use of spine fixation appears more successful in patients over 7-9 years of age,
versus patients over 9 years of age. In the older patients, the grip strength
of the screws is more reliable, due to the ability to maintain bony fixation. If the fixation is UNBALANCED (upper vs. lower) then the end with weaker fixation is more likely to fail. This is important when the caudal (below) fixation is in the iliac crests or sacropelvis, as this is a very strong fixation method. Therefore, in this case the BALANCED fixation is sacropelvic fixation caudally, and 6 pedicle screws used at the cranial side creating BALANCED fixation. If the lower foundation is to the spine, then the cranial fixation with 4 screws may be sufficient. By fixating short of the pelvis, a lot of the normal body/trunk motion is dissipated by the lumbar spine below the spine fixation. - The use of two rods is stronger than using one rod. However, the use of one rod is occasionally necessary because the spinal deformity may prevent safe placement of two rods. A child with low body mass, and hence low muscle mass may not allow a rod on the convex side. The other situation is in the spinal deformity with significant kyphosis, called kyphoscoliosis, which can preclude a rod on the convex side, especially a magnetically-controlled growing rod.
The caudal foundation options are presented here. If the fixation can stop short of the pelvis,
onto the spine, this is preferred. The risk of a surgical site infection is lower if pelvic fixation can be avoided.
If fixation needs to go to the pelvis, such as the pelvis is very tipped at an angle, then all methods of fixation are reasonable to use.
Here are the three main types of pelvic fixation:
- The left picture shows the use of a Dunn-McCarthy or “S” hook. This device rests on the top of the iliac crest and was popularized by Dr. Robert Campbell with the VEPTR
device. - The middle picture is another method of iliac crest fixation called pelvic saddles.
- The right picture is sacropelvic fixation using pedicle screw at bilateral L5 and bilateral S1 and bilateral iliac screws. This is a very strong, rigid method of fixation.
The choice of fixation method depends on multiple factors, such as patient age, diagnosis, deformity type, and surgeon training and experience.
As mentioned two rods are stronger than one, so we typically try to put in two rods.
Another obvious statement is to use bigger rods (5.5 mm vs. 4.5 mm) as they have a lower fracture rate.
What type of rods should be used? In general, the use of magnetically-controlled growing rods is preferred as this minimizes the number of surgical procedures. However, the use of traditional growing rods may be necessary due to the patient size and type of spinal deformity.
In conclusion, it is important to have shared decision-making. Ideally, the decision
of growing rods vs. posterior spinal fusion is one, which usually occurs over multiple office visits. Both approaches are reasonable and the complications, potential outcomes and need for future surgical procedures are the main drivers of the decision.