Two blog posts ago the topic of thoracic Scheuermann’s Kyphosis (SK) was presented, stopping short of discussing the surgical treatment. In this post we will show a patient who underwent correction of his SK using posterior column osteotomies (see blog post from 9-6-2020) and posterior spinal fusion (see blog post from 1-16-2022).
The two main reasons patients choose to undergo surgical correction
are:
– Back
pain. Surgery can be an option when the back pain has not responded to
nonsurgical treatments and is severe enough that the patient is unsatisfied
with their quality of life.
– Aesthetics/Appearance of the body. SK causes changes in the body, which
are viewed as unappealing, such as slouching, having a “poochy” belly and small
chest/breasts, and tendency to look down at the ground with difficulty in
looking straight ahead. Patients can
have a very negative opinion of their body, and this can negatively impact
their self-image and social interactions. We cannot underestimate, or minimize,
the impact of SK on the patients, specifically on their mental health. Body dysmorphia is real issue in SK.
What is our goal of surgery (posterior spinal fusion)?
We aim to correct the
kyphosis to be in, or very close, to the normal range of thoracic kyphosis. Not all kyphosis deformities should be
corrected into the normal range (<50 degrees) since this can increase the
risk of having a complication during or after surgery.
What are the overall risks of surgery? In spine deformity surgery,
there are two layers of risk:
– Risks
possible with any surgery on the human body
– Risks
unique to spine deformity surgery
What are the “risks possible with any surgery on the human body”?
– General anesthesia. This means patients are completely asleep
under anesthesia and are intubated having a ventilator breathe for them.
– Surgical Site Infections (SSIs). Surgery
is done through incisions on the skin. Even in minimally-invasive surgery, skin
incisions have to be made to access areas of the body. This introduces the risk of SSIs, most
commonly a bacterial infection, such as Staphylococcus aureus. This risk is
minimized by the surgical team and O.R. in many ways, such as using
intraoperative antibiotics and diligent sterile technique.
– Worsening of pre-existing medical
conditions. Heart disease, lung disease, neurologic diseases can all increase
the risk of a complication related to surgery.
What are the “risks unique to spine deformity surgery”?
– Spinal Cord Function. In spine deformity,
surgery the focus of attention is mainly on the spinal column, or the bone of
the spine. Inside the spinal column are
the spinal cord and nerve roots, and around the spinal column are blood vessels
and other organ systems. Most spinal
deformity surgeries never encounter the major blood vessels or other organ
systems, so we are more concerned with the spinal cord and nerve roots. For surgery of the thoracic and lumbar spine,
the spinal cord and nerve give muscle function and sensation in the legs and
control the bowel and bladder. It is
desirable the spinal cord and nerve roots work the same after surgery as they
do before surgery. However, during surgery the patients are under general
anesthesia so they cannot tell us if there is a problem with spinal cord
function, and cannot actively move the legs.
During surgery, the spinal cord function is assessed by an
intraoperative neuromonitoring specialist, which evaluate the electrical
signals of the spinal cord. This method
of spinal cord testing is 99.8% accurate in determining final neurologic
outcome from surgery.
– Early Movement/Migration/Pull-out of
Spinal Fixation.
– Failure of Spinal (Bone) Fusion.
– Need for Reoperation.
– Adjacent Segment Angulation/Breakdown.
– Back and Leg Pain.
*** Please note the risks of surgery just listed are some of the most
common, which may occur. This list is
not exhaustive nor inclusive of all potential complications. A discussion about complications is important
to have before surgery.
So let us go to the surgical case…….
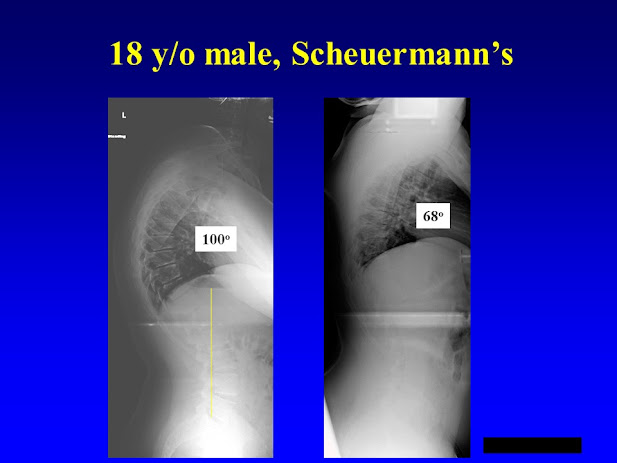
The case is an 18-year-old
male with SK. His pain is mainly over the area of his back where the red arrow
is pointing.
The left side radiograph
is the patient standing upright. On the right is him lying on his back with a
bump under the area of kyphosis, which makes him extend his back. This gives us information about his spinal
flexibility and how difficult it will be to correct his deformity. In general,
a more flexible spine makes the surgery easier, faster and safer.
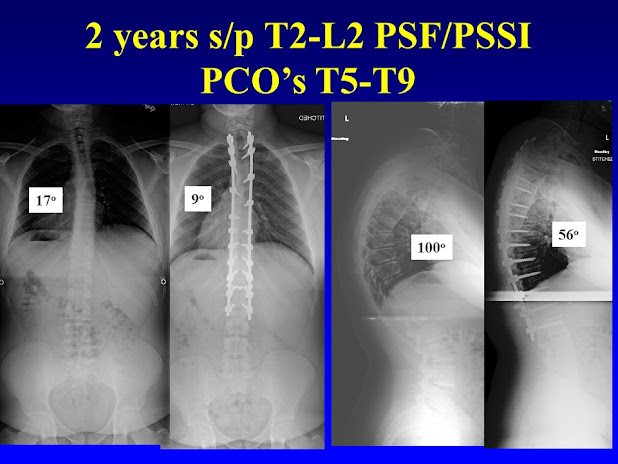
Here is the patient now
1 year after surgery. His thoracic
kyphosis is 56 degrees, which is just above the normal range. However, his overall appearance and spinal balance
is excellent and he has no back pain.
Here he is now 2 years
after surgery
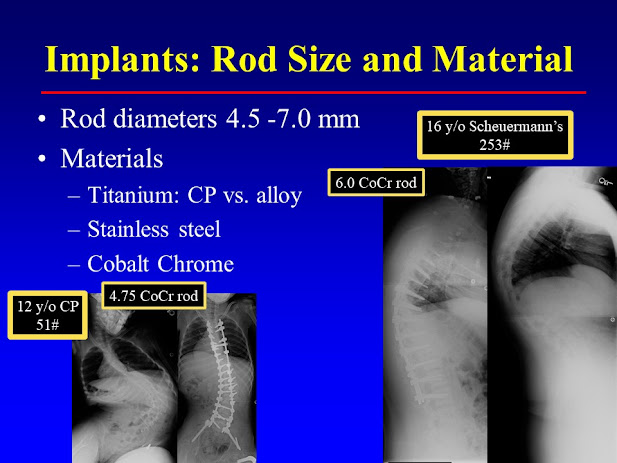
In 2022 the three most
common metals used for spinal rods in spine deformity surgery are cobalt
chrome, titanium (pure and alloy) and stainless steel. For SK surgeries, we
need to use very stiff spinal rods, such as a 6.0 mm Cobalt Chrome or 6.35 mm
Stainless Steel. Smaller, more flexible
rods will not allow us to achieve a new spine position and will not maintain
the new spine position as the spine fusion develops.